Alzheimer’s disease is a serious condition that affects the brain. It is the most common type of dementia, which means it can make it hard for people to remember things, think clearly, and even do everyday tasks. Understanding Alzheimer Facts is important for everyone, especially for families, friends, and caregivers. In this article, we will share some key facts about Alzheimer’s, explore important figures, and discuss Alzheimer Best Practices to help those affected by the disease.
What is Alzheimer’s Disease?
Alzheimer’s disease is a brain disorder that affects memory, thinking, and behavior. It usually starts slowly, with people forgetting things or having trouble remembering names. Over time, these memory problems can get worse, and it can be hard for someone with Alzheimer’s to remember where they are or what day it is.
Imagine your favorite book, where the story starts to get blurry, and you can’t remember what happened in the beginning. That’s similar to what happens to people with Alzheimer’s. Their memories fade, and they may struggle to recognize their loved ones.
Important Alzheimer Facts
Here are some important Alzheimer Facts that everyone should know:
- Prevalence: According to the Alzheimer’s Association, more than 6 million people in the United States are living with Alzheimer’s. This number is expected to increase as more people live longer.
- Age Factor: Most people with Alzheimer’s are over the age of 65. However, early-onset Alzheimer’s can occur in people in their 30s, 40s, or 50s.
- Symptoms: Common symptoms include memory loss, confusion, difficulty with problem-solving, and changes in mood or behavior. Sometimes, people may become lost in familiar places or have trouble finding the right words.
- Diagnosis: Doctors use different tests to diagnose Alzheimer’s, including memory tests, brain scans, and health assessments. If you or someone you know is having memory problems, it’s important to see a doctor.
- Cause: The exact cause of Alzheimer’s is not completely understood. However, researchers believe it involves a mix of genetics, lifestyle, and environmental factors.
- Risk Factors: Some factors that increase the risk of Alzheimer’s include age, family history, and certain health conditions, like heart disease or diabetes.
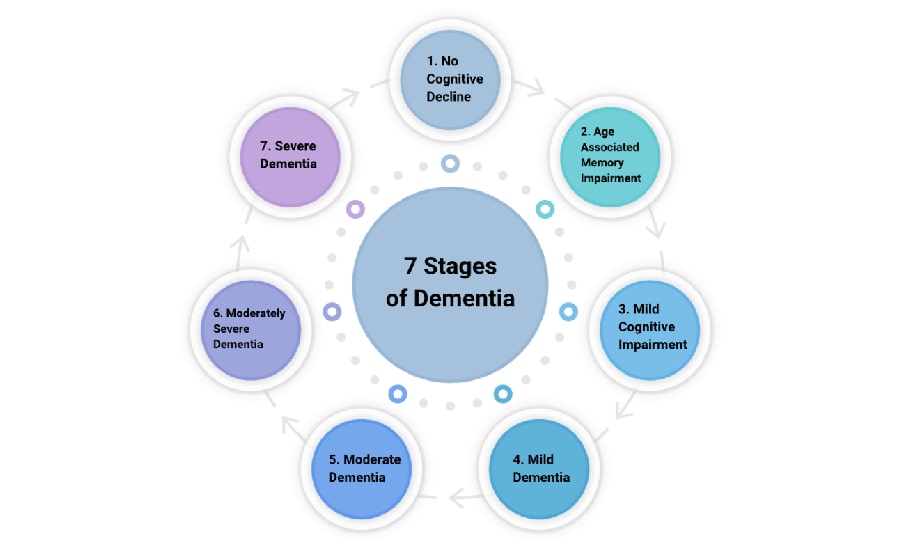
- Progression: Alzheimer’s disease progresses in stages, starting with mild memory loss and advancing to severe cognitive impairment, where the person may not be able to communicate or recognize loved ones.
- Life Expectancy: The life expectancy after diagnosis can vary, but on average, people with Alzheimer’s live about 4 to 8 years after being diagnosed. Some may live longer, while others may decline more rapidly.
Figures About Alzheimer’s Disease
Understanding the numbers behind Alzheimer’s can help us see how big of a challenge it is. Here are some important figures:
- Global Impact: Around 50 million people worldwide are living with dementia, with Alzheimer’s being the most common form.
- Economic Cost: The cost of caring for people with Alzheimer’s is enormous. In 2021, it was estimated that caring for individuals with dementia in the United States cost about $355 billion.
- Caregivers: More than 11 million people in the U.S. provide unpaid care for someone with Alzheimer’s or another type of dementia. This care can be emotionally and physically demanding.
- Death Rate: Alzheimer’s is the sixth leading cause of death in the United States. The number of deaths due to Alzheimer’s has increased significantly over the years.
Alzheimer Best Practices
Caring for someone with Alzheimer’s can be challenging, but there are Alzheimer’s Best Practices that can help make the journey a little easier for everyone involved. Here are some important practices to consider:
1. Create a Routine
Having a daily routine can provide comfort and stability for someone with Alzheimer’s. Regular schedules help them feel secure and know what to expect. Simple activities like meals, walks, and bedtime routines can be helpful.
2. Use Clear Communication
When talking to someone with Alzheimer’s, it’s important to use clear and simple language. Speak slowly and make eye contact. If they have trouble understanding, try to be patient and repeat things if needed.
3. Stay Engaged
Encourage activities that stimulate the mind and body. This could include puzzles, memory games, or even simple exercises like walking or stretching. Engaging activities can help improve mood and reduce anxiety.
4. Provide a Safe Environment
Make sure the living space is safe and comfortable. Remove any hazards, like loose rugs or sharp objects, that could cause falls or injuries. Consider using labels to help them remember where things are.
5. Be Patient and Understanding
Caring for someone with Alzheimer’s can be frustrating at times. It’s important to be patient and understand that their behavior may change due to the disease. Try to offer reassurance and support when they feel confused or upset.
6. Encourage Independence
As much as possible, encourage the person to do things for themselves. This could be simple tasks like getting dressed or making a snack. Promoting independence can help maintain their dignity and self-esteem.
7. Connect with Support Groups
Connecting with other caregivers can be very helpful. Support groups offer a chance to share experiences, gain advice, and find comfort in knowing that you are not alone. Many organizations, like the Alzheimer’s Association, offer resources and support.
Best Practice Alzheimer Care
The best care for someone with Alzheimer’s involves a mix of love, patience, and understanding. Here are some key points to remember for best practice Alzheimer care:
- Regular Check-ups: Make sure the person has regular visits to the doctor to monitor their health and adjust any medications if needed.
- Healthy Lifestyle: Encourage a healthy lifestyle, including a balanced diet, regular exercise, and good sleep habits. This can help improve overall well-being.
- Plan for the Future: It’s important to discuss future care options and make plans as the disease progresses. This might include legal and financial matters, as well as preferences for care.
- Educate Yourself: Learn as much as you can about Alzheimer’s disease. The more you know, the better you can support your loved one.
Conclusion
Alzheimer’s disease is a complex and challenging condition that affects millions of people and their families. By understanding Alzheimer Facts and recognizing the importance of Alzheimer Best Practices, we can provide better care and support for those living with this disease. Remember that every person with Alzheimer’s is unique, and the journey can be different for everyone. With love, patience, and understanding, we can help make their lives a little brighter. Whether you’re a caregiver, a family member, or a friend, you have the power to make a positive impact in their lives!